“HPV Vaccine is cancer prevention”, the CDC’s campaign slogan, is not hyperbole and represents one of the most important intervention we can do in Primary Care. Over 270,000 women died from cervical cancer globally in 2012 and 90% of them would have lived had they received the HPV vaccine at age 11.
This week’s issue of the New England Journal presents a milestone in expanding the coverage of cancers associated with the human papillomavirus (HPV).
Below is an abbreviated reprint of an editorial published in today’s Journal by Anne Schuchat.
Joura and colleagues report the results of a randomized, controlled trial of a new 9-valent HPV vaccine versus a quadrivalent HPV vaccine in more than 14,000 young women. The authors found that the new vaccine had an efficacy of nearly 97% against high-grade cervical, vulvar, and vaginal disease related to HPV types 31, 33, 45, 52, and 58. In the intention-to-treat analysis, the 9-valent vaccine was not found to be more beneficial than the quadrivalent vaccine, presumably because so many of the study participants, who were between 16 and 26 years of age, had already been infected with the five HPV types added to the new vaccine by the time of the study’s onset. The rationale for vaccination at 11 to 12 years of age is to provide protection before exposure to HPV.
What HPV researchers talk about when they talk about “coverage” is the distribution of HPV types in cancers. Earlier vaccine formulations targeted the most common oncogenic types, 16 and 18, which are responsible for about 70% of cervical cancers. The 9-valent vaccine is expected to target an additional 15 to 20% of cervical cancers and an additional 5 to 20% of other HPV-related cancers. While HPV-related cancer coverage can now expand, other types of coverage present ongoing challenges.
What many Americans talk about when they talk about “coverage” is health insurance. The HPV vaccine has been included in the Vaccines for Children (VFC) program since 2006. The program entitles uninsured children through 18 years of age to free access to vaccines recommended by the Advisory Committee on Immunization Practices (ACIP).
Since 2010, the Affordable Care Act (ACA) has required private health insurers to cover these vaccinations and has prohibited copayments or deductibles when the vaccines are delivered by an in-network provider.
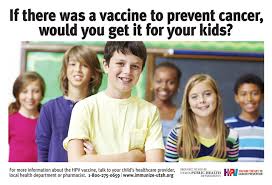
At 57%, coverage for the first dose of HPV vaccination among girls 13 to 17 years of age lags behind coverage for other vaccines recommended for children 11 to 12 years of age by approximately 20 to 25 percentage points. If teenagers were offered and accepted HPV vaccination every time they received another vaccine, first-dose coverage for HPV would exceed 90%. Even though private doctors’ offices stock vaccines, and parents and teens visiting the offices accept other immunizations, 4 of 10 adolescent girls have not even begun HPV vaccination. Formative research suggests that parents hear mixed messages about HPV vaccination; pediatricians communicate less urgency and give weaker recommendations for this vaccine. When clinicians present HPV vaccine together with tetanus–diphtheria–acellular pertussis and meningococcal vaccines and make strong recommendations, there is greater acceptance.
Decades from now oncologists will still be talking about HPV-associated cancers with thousands of new patients every year. Instead, I hope that in a few decades we will be able to tell a generation of adults who never had HPV-associated cancers or precancers that when they were teenagers, we had them covered.